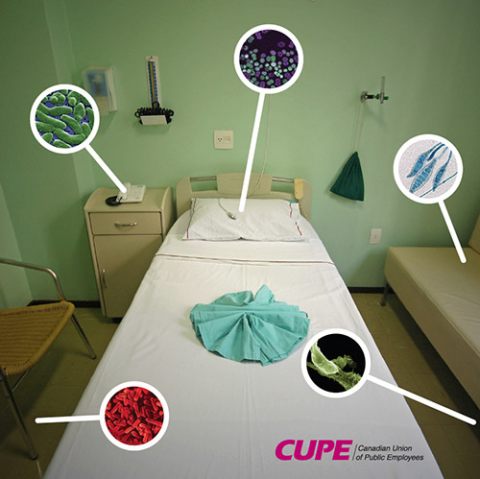
Healthcare associated infections develop in a patient as a result of their exposure to healthcare facilities or procedures. They include methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), C. difficile and other infections caused by bacteria and viruses encountered in healthcare facilities.
Rising infection rates are causing unnecessary suffering and death and are taxing the healthcare system as well as patients and families.
- Each year in Canada, more than 220,000 healthcare associated infections result in 8,500-12,000 deaths, and the rates are rising.
- One in nine hospital patients in Canada get a healthcare associated infection.
- Infections are the fourth leading cause of death in Canada.
Download the backgrounder and fact sheet below.
The incidence of methicillin-resistant Staphylococcus aureus (MRSA) in Canadian hospitals increased 17-fold between 1995 and 2006. The rate of patients contracting C. difficile increased almost five-fold between 1991 and 2003. Outbreaks of other types of healthcare associated infections are also on the rise.
The direct costs of hospital acquired infections in Canada are estimated to be $1 billion annually. On top of that are costs borne by patients and volunteer caregivers as well as program costs for home and community care.
Much of the suffering and death caused by HAIs is needless. The Canadian Committee on Antibiotic Resistance estimates that at least 30 per cent of healthcare associated infections can be prevented.
Cleaning, laundry, and other support services are a vital element of infection prevention and control strategies. Pathogens such as C. difficile, VRE, MRSA, norovirus, influenza, and severe acute respiratory syndrome (SARS) associated coronavirus can survive in the healthcare environment for extended periods of time, even months. In fact, these infections are inherently well adapted to survive in dust and on floors, bedrails, telephones, call buttons, curtains and other surfaces. Washing hands is important, but if bacteria and viruses are not eliminated from the environment, hands will quickly become contaminated again.
“Breaking the chain of infection” requires well-resourced, well-trained, and stable in-house healthcare teams attacking all of the links of transmission; sufficient beds, equipment and staff to achieve best practice occupancy rates; modern high-quality infrastructure and equipment, and; standardized procedures, monitoring and public reporting.
Solution One: More healthcare cleaning and infection control staff, with proper training and continuity
- Hospital spending on support services in Canada fell from 26 per cent of total budgets in 1976 to 16 per cent in 2002. Most of those cuts applied to staffing, with cleaning departments taking a major hit.
- Clinical studies and audits have linked healthcare associated infection outbreaks with understaffing, increased workload, high turnover, and inadequate training.
- Hospitals in Canada and Europe have demonstrated that investment in more cleaning and infection control staff, training and workforce stability has brought infection rates down.
Solution Two: More rigorous cleaning and proper supplies
- Studies and guidelines from infection control specialists recommend intensive cleaning with proper materials to eradicate healthcare associated infections.
Solution Three: Stop and reverse contracting-out
- Contracting-out leads to cuts in staff, lower wages, fewer benefits, higher turnover rates, less training, and a rift between clinical and support services. High turnover, poor training, and the breakdown in team work are factors in HAI outbreaks.
- Investigations into HAIs in the United Kingdom have found that infection rates spiked after contracting-out and cuts in hospital support services. Scotland and Wales have decided to halt and reverse the privatization of hospital cleaning as part of aggressive campaigns against HAIs.
Solution Four: Reduce occupancy rates
- Overcrowding and rapid turnover between patients seriously hamper infection control procedures and are a major factor in infection outbreaks.
- Across Canada, hospital beds were cut by 36 per cent between 1998 and 2002, and bed occupancy reached 95 per cent by 2005.
- The Netherlands, which has one of the lowest rates of MRSA, had a bed-occupancy rate of 64 per cent in 2005.
Solution Five: Mandatory standards, monitoring and public reporting
- Healthcare facilities should adopt strict microbiological standards to replace the current standard that rooms and equipment “appear clean.” In a UK study, researchers found that 90 per cent of the wards that had been declared clean in a visual assessment were shown by microbiological testing to have an unacceptable load of microorganisms.
- Mandatory public reporting of healthcare associated infection rates and deaths by healthcare facilities and by departments are also necessary to improve transparency and accountability.

